Table of Content
- Which KPIs Should Your Home Health Care Agency Track?
- Alignment of quality indicators with broader home care reforms
- Events
- What Parents Have to Say: Content and Actionability of Narrative Comments from Child HCAHPS Survey
- Financial KPIs
- Profit
- Patient consent for publication
- Adjusting for Patient Characteristics to Compare Quality of Care Provided by Serious Illness Programs
Profit is the financial gain you keep when you subtract all the expenditures from revenue. You can calculate it by subtracting direct and indirect expenses from all revenue earned. Direct costs can include staff salaries and various material purchases, while indirect costs include rent, utilities, etc. Tracking your monthly expenses can help you set your priorities, achieve your goals, and protect your business from cash flow challenges. You can analyze it from a monthly or yearly standpoint, depending on the purpose of your exploration.
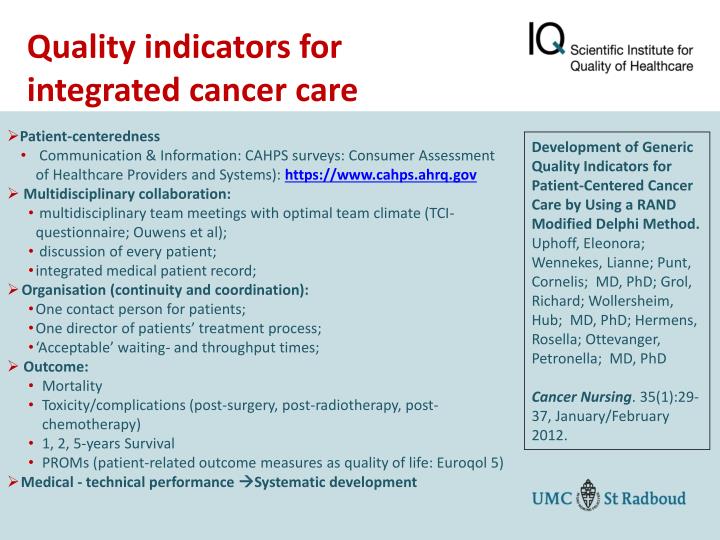
Process measures are derived from data collected in the OASIS submitted by home health agencies and are calculated using a completed quality episode that begins with admission to a home health agency and ends with discharge, transfer to inpatient facility or sometimes death. Measures based on OASIS data are calculated using a completed episode of care that begins with admission to a home health agency and ends with discharge, transfer to inpatient facility or, in some cases, death. We believe it would be extremely useful to define a reasonable size for an indicator set in any particular setting. New Jersey's local and county health departments are community-based public health service and a first point of contact for questions about public health services or health conditions. We interviewed 105 practice leaders from 294 sampled practices and used content analysis to identify themes about uses of patient experience data for practice improvement during PCMH transformation.
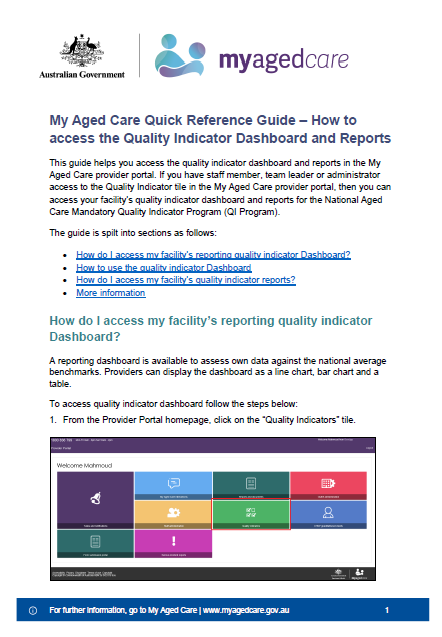
Which KPIs Should Your Home Health Care Agency Track?
HCQA applies these Quality Indicator tools to the New Jersey inpatient discharge data to come up with data that measure healthcare quality. The data help hospital administrators and DOH to identify potential areas of concern that may need further investigation. Increasingly, tools and surveys are employed to determine current and optimal levels of health care service and performance, and ultimately to improve the levels for each. RAND helps policymakers, health care leaders, and practitioners determine cost-effective and accurate ways to measure the quality of health care being provided, and then recommends ways to improve the level of health care quality. KPIs need to address all aspects of a business, from the quality of care and client conversion to HR, marketing, and finance.
To calculate it, divide the number of clients admitted by the total number of people who made an inquiry about your services in the same period. If the client turnover is significant, it might imply poor client satisfaction and the low quality of the service provided. You can calculate it by dividing the number of all active clients during a time period by the number of months care was provided.
Alignment of quality indicators with broader home care reforms
By tracking the following key performance indicators for home health care, you can identify the problems early, and take appropriate measures. To keep your agency's performance at a high level, you need to ensure that the services you’re providing are being delivered according to your client’s personal needs, at the right place, and at the right time. Below you will find four key performance indicators in healthcare that fall into this section, that you might benefit from tracking. In accordance with Government decision to align the introduction of quality indicators with broader home care reforms, work of the consortium has refocused to identify, assess and deliver an operational framework for quality indicators and CEQOL measures in a new in-home aged care program. Our analyses provide evidence of the feasibility, reliability, and validity of proposed survey-based measures to assess the quality of home-based serious illness care from the perspective of patients and their families. Regarding key performance indicators for home health care, they should cover all key areas like overall client satisfaction, on-time client visits, employee retention, reporting, and billing.
You can use this KPI to measure client satisfaction - if it is above average, this KPI suggests that the agency is most likely providing quality care and is successful in retaining its clients. Besides their obvious rationale - the need to measure data in areas critical to success, there is another crucial reason for tracking we mustn’t forget - their human effect. Percentage of patients reporting that home health providers talked with them about their medications and pain.
Events
At the same time, your team will understand that KPIs hold them accountable for meeting their performance goals. The only way agencies can confirm that their business objectives are being fulfilled is by tracking and measuring their performance. Tightening budgets and keeping up with ever-evolving regulations, policies, and processes in this dynamic industry have put a lot of pressure on home health care agencies. The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. The RAND Corporation is a research organization that develops solutions to public policy challenges to help make communities throughout the world safer and more secure, healthier and more prosperous. This issue brief describes challenges and opportunities related to measuring, reporting, and monitoring the quality of HCBS sponsored by Medi-Cal.
This paper presents evidence that the quality of health care interactions changed in important ways during the early months of the Covid-19 pandemic. We surveyed children's hospital leaders and staff about their use of Child HCAHPS for QI, including measures from other studies. We compared scale and item means for leaders and staff and compared means to other studies. In 2008–2017, 15–18% of U.S. primary care practices sought or maintained patient-centered medical home recognition. We interviewed a sample of 105 of these practices to determine why patient experience surveys were chosen. Depression, PTSD, traumatic brain injury, and substance use disorders interfere with veterans' employment, family life, community engagement, and well-being.
We’ve chosen this set of four financial key performance indicators for home health care because they are the most critical to understanding the overall health of your business. If you monitor these metrics regularly and use them to guide your actions, it will put you in control of your home health care agency to achieve the results you want. Indeed, key performance indicators for home health care are most effective when the entire staff is familiar with them and is using this data to improve their performance. If an agency is working without tracking key performance indicators in healthcare, it can create vagueness around its performance. In addition, it will soon become challenging for the agency to compare its progress over different periods. The CAHPS Home Health Care Survey addresses the experiences of home health care patients with agency staff.

Technical documentation for calculating process measures can be accessed via the link to Technical Documentation of OASIS-Based Measures in theDownloadssection below. New Jersey is home to over 2,000 licensed hospitals, nursing homes, and medical care facilities. The New Jersey Department of Health works to ensure that citizens receive appropriate levels of care in every regulated facility.
However, due to the COVID-19 Public Health Emergency HHQRP data submission requirements for the Q4 2019, Q1 2020, and Q quarters were exempted. The missing data for Q and Q will impact what is displayed on Care Compare; therefore, public reporting of home health agencies' data will freeze after the October 2020 refresh. This means that following the October 2020 refresh, the data publicly reported will be held constant for all refreshes in 2021, including October 2021. You can find detailed specifications for the claims-based measures in theDownloadssection below.
Percentage of patients reporting that home health providers treated them as gently as possible. The development of measures for home health is in the early stages, but several measures have been endorsed by NQF and are being reported. Here are some examples of measures that would be appropriate for reporting to consumers and are currently included in the Centers for Medicare & Medicaid Services’ (CMS’) Home Health Compare Web site. The Patient Safety Indicators provide information on potential in hospital complications and adverse events following surgeries, procedures, and childbirth. PSIs can be used to help hospitals identify potential adverse events and assess the incidence of adverse events and in hospital complications. On February 7, 2022, the RAND Corporation convened a Technical Expert Panel web meeting to gather input about the potential development of a measure to capture value-based care arrangements Medicare Advantage organizations have with their contracted providers.
A set of standards can help identify providers who serve veterans and deliver high-quality care. Such analysis can help you determine whether there is anything in the process that makes the prospective clients give up using your agency's services. By tracking KPIs for your primary goals, you will know if your team is reaching home health productivity benchmarks, and you can implement incentives based on their achievements.
On the other hand, annual revenue is significant for determining whether you are paying yourself and your staff properly. Most organizations set objectives, and KPIs are used to show the direction an organization is moving into by providing objective and comparable data, expressed by numbers. Variations in quality of Home Care between sites across Europe, as measured by Home Care Quality Indicators. Quality of care in European home care programs using the second generation interRAI Home Care Quality Indicators . HHS is committed to making its websites and documents accessible to the widest possible audience, including individuals with disabilities.

No comments:
Post a Comment